Girişimsel olmayan aritmi
Noninvasive arrhythmia
[P-241]
[P-241]
İskemik inme için yüksek riske sahip atriyal fibrilasyonlu hastalar
yeterli oral antikoagülan tedavi almamaktadır
Patients with atrial fibrillation who have high risk for ischemic
stroke do not take adequate oral anticoagulation
Faruk Ertaş, Halit Acet, Çayan Çakır, Ümit Yuksek, Zehra İlke Akyıldız,
Nihan Kahya Eren, Cem Nazlı, Asım Oktay Ergene
Faruk Ertaş, Halit Acet, Çayan Çakır, Ümit Yuksek, Zehra İlke Akyıldız,
Nihan Kahya Eren, Cem Nazlı, Asım Oktay Ergene
Atatürk Eğitim ve Araştırma Hastanesi, İzmir
Atatürk Training and Research Hospital, İzmir
Aim: Atrial fibrillation (AF) is the most common arrhythmia seen in clinical settings. One of the most
important complications of AF, creating high mortality and morbidity, is ischaemic stroke.
Anticoagulation is an accepted teatment of AF to prevent thromboembolism. In our study, we aimed
to detect the prevalence of adequate oral anticoagulation (OAC) in AF patients whose ischaemic
stroke risk is high.
Method: Between November 2007 and May 2008, 200 consecutive patient presenting with AF to our
cardiology clinic were screened. Patients are classified according to their ischaemic stroke risk.Risk
for ischaemic stroke is determined according to the ‘2006 ACC/AHA/ESC Atrial Fibrillation’ guideline ischaemic stroke risk strafication. According to this stratification, risk groups are classified as
follows;
1) High-risk group: Ischaemic stroke, transient ischaemic stroke attack or systemic embolus history,
mitral stenosis, mechanical prosthetic valve, patients having more than one of the intermediate risk
factors.
2) Intermediate-risk group: >75 years of age, diabetes, hypertension, ejection fraction (EF)< 35
3) Low-risk group: 65-74 years of age, coronary artery disease, thyrotoxicosis
Among 200 patients; 176 high risk patients were enrolled to our study. Patients under OAC were
eveluated for adequate anticoagulation with the determination of INR values. Appropriate target INR
for every patient was defined as adequate anticoagulation according to ‘2006 AHA/ACC/ESC Atrial
Fibrillation’ guideline.
Results: Six patients (3%) were in low-risk group; 18 patients (9%) were in intermediate-risk group
and 176 patients (88%) were in high-risk group. One hundred seventy-six (woman, n=114, 57%; men,
n=86, 43%) high risk patients were enrolled to our study. Nine-teen patients from high risk grup were
excluded;11 patients (6.25%) due to low socioeconomical status inducing non-compliance to OAC
and 8 patients (4.54%) due to medical contraindications.One hundred fifty-seven high risk patients
were included in the study. One hundred six (67.51%) of them were not on any OAC; 51 (32.49%) of
them were using OAC. Among 51 patients using OAC, 14 (27.46%) had reached the appropriate
target INR values according to the guidelines; whereas 37 (72.54%) had not reached the appropriate
target INR values. Among all high risk AF patients, 23.56% of them had not reached the appropriate
target INR values.
Discussion: Although there are outstanding studies showing that OAC treatment prevents ischaemic
stroke;only one third of AF patients under high risk of ischeamic stroke is using OAC treatment. On
the other hand, only one third of these patients has reached the appropriate target INR values. In our
study, which we recorded real world data, contraindications for OAC can not explain our results. We
propose that, not being under OAC treatment may be related to patient-based individual limitations of
OAC treatment use or indifference to the treatment based on patient’s risk.
[P-242]
[P-242]
Atrial senkronize ventriküler pacing yapılan hastalarda kalp hızı
değişkenliği ve kalp hızı türbülansı
Heart rate turbulence and heart rate variability in patients with
atrial synchronous ventricular pacing
Harun Kılıç,1 Özlem Karakurt,1 Ramazan Akdemir,1 Mehmet Doğan,1
Asuman Yeşilay,1 Göksel Çağırcı,1 Sadık Açıkel,1 Hüseyin Gündüz2
Harun Kılıç,1 Özlem Karakurt,1 Ramazan Akdemir,1 Mehmet Doğan,1
Asuman Yeşilay,1 Göksel Çağırcı,1 Sadık Açıkel,1 Hüseyin Gündüz2
1
Ankara SB Dışkapı Yıldırım Beyazıt Eğitim ve Araştırma Hastanesi, Kardiyoloji
Kliniği, Ankara; 2Abant İzzet Baysal Üniversitesi Bolu Tıp Fakültesi Araştırma ve
Uygulama Hastanesi Kardiyoloji Anabilim Dalı, Bolu
1
Department of Cardiology, Ankara SB Dışkapı Yıldırım Beyazıt Training and
Research Hospital, Ankara; 2Department of Cardiology, Bolu Medicine Faculty of
Abant İzzet Baysal University Training and Research Hospital, Bolu
Giriş: Kalp hızı değişkenliği (HRV) ve Kalp hızı türbülansı (HRT) kalp hastalarının bazı gruplarında bağımsız ve güçlü bir mortalite belirleyicisidir. Pacing yapmanın kalp otonomik sistemi
üzerine olumsuz etkisi vardır. Bu çalışmada amacımız atrial senkronize ventriküler pacing (VDD)
yapılan hastalarda HRT ve HRV’yi araştırmaktır.
Metod: Çalışma grubu 12 kontrol ve 12 normal sinus fonksiyonlu, yüksek dereceli atrioventriküler blok nedeniyle VDD takılmış organik kalp hastalığı olmayan hastalardan oluşmaktadır. HRT ve
HRV, 24 saatlik holter kaydı ile incelendi.
Sonuçlar: HRV parametreleri açısından iki grup arasında istatiksel olarak önemli fark yoktu. HRT
parametreleri karşılaştırıldığında türbülans başlangıcı (TO) kardiyak pace grubunda kontrol grubuna göre anlamlı olarak daha yüksekti (2.729 ± 8.818 vs -1.565± 8.301, p=0.006), fakat türbülans
eğimi (TS) açısından iki grup arasında anlamlı fark yoktu (11.166 ± 10.034 vs. 31.675 ± 28.107,
p=0.68). Anormal TO’lu hasta sayısı pace grubunda kontrol grubuna göre anlamlı olarak daha
fazla idi (9 vs. 2, p=0.004).
Tartışma: Atriyal senkronize pacing yapmanın otonom fonksiyon üzerine olumsuz etkileri vardır.
Değişmiş ventriküler depolarizasyon otonom fonksiyonlarda bozulmaya yol açmış olabilir.
Kontrol ve VDD hastalarında HRV farkı bulunmasa da, TO ve anormal TO’lu hasta sayısı VDD
hasta grubunda anlamlı olarak daha fazla idi. VDD hastalarında, TO otonomik cevabın invazif
olmayan şekilde değerlendirilmesinde en uygun yöntem olabilir.
Background: Heart rate turbulence (HRT) and heart rate variability (HRV) have been shown to
be independent and powerful predictors of mortality in a specific group of cardiac patients. Pacing
has unfavorable effects on autonomic function. Our aim is to investigate autonomic responses to
atrial synchronous ventricular pacing (VDD) by evaluating HRT and HRV parameters.
Methods and Results: The study groups comprised 12 control and 12 patients without organic
heart disease and with normal sinus function who were implanted with a permanent VDD pacing
system for high degree atrioventricular block. The HRV and HRT analysis were assessed from a
24-hour Holter recording. There was no statistically significant difference between the two groups
for HRV parameters. When HRT parameters were compared, Turbulence Onset was significantly
higher in cardiac paced group than the controls group (2.729 ± 8.818 vs -1.565± 8.301, p=0.006),
but no statistically significant difference was found between the two groups for Turbulence Slope
(11.166±10.034 vs. 31.675±28.107, p=0.68). The number of patients who had abnormal HRT
onset was significantly higher in the paced group than controls (9 vs. 2, p=0.004).
Conclusion: Atrial synchronous pacing has unfavorable effects on autonomic function. Altered
ventricular depolarization sequence may lead to changes in autonomic response. Although we
found no difference in HRV parameters between control and VDD patient group. The HRT onset
and number of patients with abnormal HRT onset was significantly higher in VDD patients. HRT
onset can be a better way of non-invasive autonomic response predictor in VDD patients.
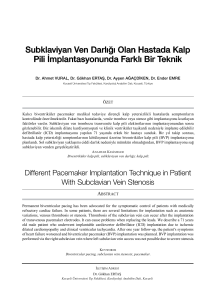
Şekil 1. Kalp hızı türbülansı (HRT) örneği.
216
Fig 1. Example of heart rate turbulence.
Türk Kardiyol Dern Arş 2008, Suppl 2